
Waystar
78 Case Studies
A Waystar Case Study
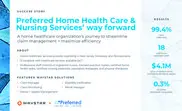
Preferred Home Health Care is a home healthcare provider serving New Jersey, Delaware, and Pennsylvania with 12 locations that delivers 24/7 clinical and non-clinical care. Facing inefficient claim processing, high paper-claim volume, slow payer enrollment and clearinghouse issues that delayed payments and tied up staff time, Preferred Home Health Care partnered with Waystar and adopted Waystar’s claim and payment management tools (including Claim Manager, Claim Monitoring, Denial + Appeal Management, Eligibility Verification, and Remit Manager).
Waystar streamlined claim submission, increased electronic payer connections, accelerated enrollment, and provided ongoing support and reporting to remove manual work and surface payer trends. As a result, Preferred Home Health Care achieved a 99.4% clean claim rate, saved 18 staff hours per week, recovered $4.1M in rebilled claims improperly denied by payers, and reduced paper claims to 0.3%, improving cash flow and operational efficiency with Waystar.

Tonya Lukas-Hallman
Billing Manager